Frequently Asked Questions: Prior Authorization Repetitive Scheduled Non-Emergent Ambulance Transports
Question 1: Is there a Centers for Medicare & Medicaid Services (CMS) form we have to use for Prior Authorization (PA) requests?
Answer: CMS does not have an official form or cover sheet. However, Palmetto GBA has created a form that can be accessed under the Forms tool on the Palmetto GBA websites for Jurisdictions J and M. Additionally, providers registered for Palmetto GBA's eServices can submit these requests electronically via the secure portal.
Question 2: Where can we obtain information from the last CMS Ambulance Open Door Forum call?
Answer: Information from the last CMS Ambulance Open Door Forum call is or will be available at Open Door Forum Podcast and Transcripts.
Question 3: Who should obtain Prior Authorization?
Answer: Because ambulance payments are made to the billing provider, it is the ambulance provider's responsibility to obtain necessary documentation to support ambulance transportation coverage.
Question 4: My request was non-affirmed. How am I able to find out why?
Answer: For non-affirmed determinations, the code provided in the reason field of the decision (i.e., AMB6Z) can be found on the Non-Affirmed Code Crosswalk: Prior Authorization Request. The crosswalk is a table that lists the non-affirmation reason codes and their descriptions and is available on the Palmetto GBA website. These are the reasons why the request is not fully approved or affirmed. Providers are also contacted for any non-affirmed requests to educate regarding the non-affirmation reason code.
Question 5: How will I know how many transports are authorized?
Answer: For Affirmed determinations, the number of transports approved will be listed in the Reason field of the decision letter.
Question 6: If we send in a Prior Authorization request for transports that have already been authorized under another ambulance provider who stopped providing the transports without notifying anyone, how will that be handled?
Answer:
- An affirmative prior authorization decision does not follow the beneficiary
- Only one ambulance supplier is allowed to request PA per beneficiary per time period. If the initial supplier cannot complete the total number of prior authorized transports, the second supplier should submit a PA request to their Medicare Administrative Contractor (MAC).
- The PA request must include the required documentation in the submission
Question 7: Do I use the same Unique Tracking Number (UTN) if I get authorized for a subsequent period because my patient requires transport beyond the initial 60-day period?
Answer: You will be given a new UTN with each Prior Authorization 60-day period.
Question 8: The Prior Authorization is for 52 trips and only 40 trips were used in the 60-day period. Can we still get the other 12 trips?
Answer: No. You will need to request another PA since the initial one is expired. Claims submitted after the expiration of the PA will suspend and an Additional Documentation Request (ADR) letter will be sent to the supplier prior to payment determination.
Question 9: Would my patient who goes to dialysis and wound care use one Prior Authorization (PA) request?
Answer: Yes. Only one PA request is required per 60-day period. However, if additional transports are needed beyond 80 within the 60-day period a subsequent PA request should be submitted.
Question 10: What if the Physician Certification Statement (PCS) expires during the Prior Authorization period?
Answer: Providers are responsible for ensuring a valid PCS is always on file and for any related tracking. The provider would need to ensure that a valid PCS is on file to pick up when the previous PCS expires.
Question 11: Does this Prior Authorization (PA) model apply Medicare Advantage (MA) Plans such as Care Improvement Plus?
Answer: This particular model is not for MA Plans. However, MA plans may require PA. Contact the specific MA plan for more information.
Question 12: The patient was transported for an X-ray in addition to dialysis, so we think the destination may need to be changed on an affirmed Prior Authorization (PA). How do we handle this?
Answer: If the Medicare beneficiary has already met the criteria to establish that their ALS or BLS non-emergent transports are repetitive and a claim for a non-repetitive transport (i.e. X-ray) is submitted, this transport would count towards their number of affirmed transports. Submit the Unique Tracking Number (UTN) on the claim for the X-ray transport. This will not permit the number of affirmed transports on that UTN to be exceeded. If the UTN is not submitted on the X-ray claim, an Additional Documentation Request (ADR) will be sent, and the claim will be reviewed once the documentation is received.
Question 13: If there is a timing issue with getting the information from a patient’s provider, how long does the provider have to get the needed information?
Answer: If a prior authorization has not been requested before the fourth round trip, claims will be subject to pre-payment medical review, which will allow additional time to obtain the needed information.
Question 14: How long does the Medicare Administrative Contractor (MAC) have to perform their initial review?
Answer: MACs will issue Prior Authorization (PA) determinations for requests submitted with all of the necessary information within 10 business days of the initial or resubmission request.
Question 15: Are hospital-based ambulances (hospital-owned ambulances) allowed to participate in the demonstration?
Answer: No.
Question 16: We have an established dialysis patient with a current Physician Certification Statement (PCS). We now need to submit a PCS with the Prior Authorization (PA) request but the physician does not want to sign far ahead.
Answer: The documentation requirements have not changed. The Physician Certification Statement (PCS) is valid for 60 days. The ambulance supplier should submit the PCS that is valid for the start date provided on the PA request. A valid PCS should be maintained throughout the approval period even if the PCS expires prior to the end of the 60-day PA period.
Suppliers are strongly encouraged to build relationships with the management teams they serve (Dialysis Centers, SNFs, etc.) and to educate them on the new process.
Question 17: We need the PTAN of the physician who is signing the Physician Certification Statement (PCS). How do we get that?
Answer: The ambulance supplier will need to obtain that from the physician or the physician’s office who signed the PCS. Please note this is not a required field on the Prior Authorization (PA) Request form.
Question 18: What happens if the signing provider refuses to give the PTAN number?
Answer: Providers are encouraged to submit the PTAN, but it is not a required field for claims processing as we realize this may be an issue.
Question 19: The patient is discharged to home from the hospital and needs dialysis the next day (will be repetitive). We would only have 24 hours to obtain the Physician Certification Statement (PCS) for the Prior Authorization (PA)? We could make several transports within 10 days while we are waiting for PA.
Answer: The claims processing system will not look for the PA Unique Tracking Number (UTN) until the fourth round trip claim is received. If the PA has not been received by the fourth transport, it does not mean the claim won’t be paid. It means the claim will be stopped for prepay review and documents will be requested by Additional Documentation Request (ADR) letter, which will give the supplier time to obtain the PCS. Please keep in mind that a PCS is only valid for claims with dates of service on or after the date the physician signs the PCS. Claims for dates of service prior to the date the physician signs the PCS will likely be denied.
Question 20: Can a checklist be provided so that ambulance providers can make certain that coverage has been met and that all necessary documentation is met?
Answer: The clinicians will review the Prior Authorization (PA) request against all requirements for scheduled, repetitive non-emergent ambulance transports. All specific reasons for non-affirmation (non-approval) are provided in a crosswalk table format. This crosswalk table is available to assist providers on the Ambulance Prior Authorization (PA) webpage. This crosswalk contains non-affirmation reason codes and their descriptions.
Question 21: If I am an ambulance company and I use a third party billing company, who is responsible for getting documentation for Prior Authorization (PA)?
Answer: If a supplier chooses to use a third party biller, it is between the provider and the biller as to who will submit the PA.
Question 22: How can we submit our request for Prior Authorization (PA)?
Answer: Palmetto GBA encourages providers to submit the request using the Palmetto GBA eServices, however you may also send via mail, fax, or esMD. Please only submit your request via one of these methods. Submitting multiple duplicate requests may slow down the process.
Question 23: How will the provider be notified of the decision?
Answer: Palmetto GBA will mail the response to the address provided on the Prior Authorization (PA) request form. It will also be faxed if a number is provided on the PA request form.
Question 24: If the ordering provider gives us their PTAN and NPI, do we have to ask for it each time or can we use what was given to us from a prior certification period?
Answer: You may use the numbers from a prior certification as long as it is the same provider currently certifying the new period.
Question 25: What if a patient uses a different ambulance supplier when discharged from the hospital?
Answer: This is typically a one-time service and would not be repetitive, so it would not require Prior Authorization (PA). If the patient continues to use that supplier for their repetitive transports, the new supplier will need to submit a PA request.
Question 26: Is there a separate form for Railroad Medicare?
Answer: This document is for Part B Medicare, which is a separate contract from Railroad Medicare. Please refer to Railroad Providers – Ambulance Prior Authorization.
Question 27: How do we know if the date of service falls within the 60-day period?
Answer: The 60-day period is 60 days from the start date provided by the supplier on the Prior Authorization request form.
Question 28: The ambulance used for the transport is equipped for ALS, so isn’t that what we should submit?
Answer: No. The service the patient needs is what determines the level of service submitted.
Question 29: Is Prior Authorization (PA) a guarantee of payment?
Answer: The ambulance supplier will know before the service is rendered whether Medicare will pay for the service. If the PA is affirmed, we will affirm (i.e., approve) up to the number of affirmed transports within that 60-day period. Then another PA request must be submitted.
Question 30: Physicians are indicating they do not want to provide additional documentation. What can we do?
Answer: The requirement for a physician certification statement is not a new requirement. The documentation requirements are not changing. Prior authorization simply requires that documentation is submitted earlier in the process. Additionally, ambulance suppliers can share the CMS Ambulance Prior Authorization Physician/Practitioner Letter (PDF) with physicians and other entities to help ensure that they obtain the necessary documentation in a timely manner.
Question 31: Can the Provider Contact Center (PCC) give me any additional information about my Prior Authorization (PA) request?
Answer: The PCC can give suppliers the status of a PA request. Ambulance suppliers will need to track the number of transports that have been affirmed, the start date and the number of transports they have already provided. Because claims can be at various stages in the claims processing system, the PCC will not be able to determine how many of the transports are remaining.
The Provider Contact Center will not be able to tell suppliers if another supplier already has a PA on file for the beneficiary. The supplier will need to work with the beneficiary, representative, nursing home, etc. to coordinate who is transporting the patient.
Question 32: I have a beneficiary who needs BLS on the way to dialysis and occasionally will require ALS on the return trip. How do I handle this?
Answer: Submit a Prior Authorization (PA) Request form for the BLS transport along with documentation to support the medical necessity. As this is how the beneficiary is typically transported. Should you later determine that the beneficiary will need an ALS transport, you may either submit a PA request for ALS which must include the order or Physician Certification Statement (PCS) documenting the need for ALS transport, or you may submit the claim which will generate an Additional Documentation Request (ADR) letter. If you choose to submit the claim, the transport will not be counted towards your affirmed number of BLS transports. Submitting the claim is encouraged if only one ALS transport is anticipated.
Question 33: What is the esMD document type for esMD submission?
Answer: Suppliers should submit a code of 81 for esMD submission of Prior Authorization requests.
Question 34: The number of trips is a required field on the Prior Authorization (PA) Request form, but we are not sure if the beneficiary will need 60 trips or the full 80. What do we place in that field?
Answer: Because the PA model is for scheduled, repetitive transports suppliers should have an idea of the number of transports that will be necessary in the 60-day period. Once into the 60-day period if the supplier determines that additional transports are needed prior to the end of the affirmation period, then the supplier should submit another PA request.
Question 35: Does the beneficiary receive a copy of the decision letter?
Answer: The beneficiary will receive a copy of the decision letter.
Question 36: Is the signature of a nephrologist accepted on the Physician Certification Statement (PCS)?
Answer: For non-emergent, scheduled, repetitive ambulance services, the order/PCS must be obtained from the beneficiary’s attending physician. If their attending physician is a nephrologist, then their signature is acceptable.
Note: Please remember that the Prior Authorization physician signature must match the Physician signature on the PCS.
Question 37: The patient is discharged from the hospital with an order for repetitive transports that begin within 48 hours of discharge. We provide the four initial transports right away within a few days. The Prior Authorization (PA) request takes ten business days to come back and we have provided more than the initial four transports. Can we submit this as an expedited PA request?
Answer: If the transports are for dialysis only:
- These are typically ordered on a Monday – Wednesday – Friday or Tuesday – Thursday – Saturday rotation
- If the patient is only using repetitive trips for dialysis, they should have all the documentation in order prior to leaving the hospital
- If dialysis begins on day two, the fifth round trip should be around day eight after discharge. You should receive the decision on the PA request by the 10th business day.
- You would also have the option of providing the service, billing it and receiving an Additional Documentation Request (ADR). If the transports meet medical necessity requirements, they should be allowed
- Fax and esMD submission will achieve faster turn-around time. Requesting the decision by fax is also an option on the PA request form.
If the transports are also for something else, such as wound care:
- It is anticipated that wound care is managed in the home and requires only periodic clinic appointments for debridement, wound management, infection types of services. In this situation an expedited request would not be necessary.
Question 38: If patient is in the middle of a Prior Authorization (PA) period for dialysis and they now need wound care on the days they are not going to dialysis, do we need to submit an additional PA request so a separate authorization can be on file for the wound care?
Answer: You do not need to submit a separate PA request for a different diagnosis. If you determine that the beneficiary may run out of affirmed transports prior to the end of the 60-day period, submit another PA request indicating the need for additional transports.
Question 39: The Prior Authorization (PA) that is affirmed for 20 round trips and we learned that the patient needs more. Do I have to submit a new PA?
Answer: Yes, a new PA needs to be submitted for the additional transports.
Question 40: Is there any information other than the Unique Tracking Number (UTN) I need to submit in the Prior Authorization field (the 2300 — Claim Information loop in the Prior Authorization reference (REF) segment, where REF01 = “G1” qualifier and REF02 = UTN)?
Answer: No, only the UTN should be entered. Palmetto GBA will reject claims when the information entered is not applicable to the intended use of these fields. Populating these loops and segments for other purposes is incorrect.
Note: A CMS system update has been implemented that directs that for submission of electronic claims, the UTN must be submitted in the 2300 Claim Information loop in the Prior Authorization reference (REF) segment where REF01 = “G1” qualifier and REF02 = UTN. A UTN submitted in this loop applies to the entire claim unless it is overridden in the REF segment in the 2400 Service Line loop.
Applicable rejections will appear on remittance notices with:
- CARC 15 — The authorization number is missing, invalid, or does not apply to the billed services or provider
- Remarks codes:
- N704 — Alert: You may not appeal this decision but can resubmit this claim/service with corrected information if warranted or
- N517 — Resubmit a new claim with the requested information
- Remarks codes:
Question 41: What if the patient changes ambulance suppliers in the middle of an affirmed 60-day Prior Authorization (PA) period?
Answer: The second ambulance supplier should submit a PA request with the required documentation. Palmetto GBA will look at data on a post pay basis to identify any transports that were submitted for reimbursement and not actually provided.
Question 42: The hospital set the patient up on dialysis with transports by another ambulance supplier. Now the beneficiary needs wound care as requested by the skilled nursing facility. If both we and the supplier providing the dialysis transports submit Prior Authorization (PA) request forms, which PA will be affirmed?
Answer: Each supplier should request Prior Authorization (PA). Data analysis will be conducted periodically with the possibility of post-pay review to ensure services are medically necessary and not duplicative.
Question 43: How do we know if a beneficiary has any open 60-day Prior Authorization (PA) periods with other suppliers? Can we see this in eServices?
Answer: There is no process for checking this currently. Please submit a PA request form as appropriate.
Question 44: What if the only destination for the transports on an affirmed Prior Authorization has changed (different from question above because destination not added and original destination not used at all anymore). How do we handle this?
Answer: Suppliers should maintain all documentation to support their documentation and billing practices. No notification to the MAC is required in this situation.
Question 45: When is the start of a Prior Authorization (PA)?
Answer: The start date is determined by what the supplier submits on the PA request. That date should be the date of the first transport.
Question 46: In the modifier 1 field on the Prior Authorization (PA) Request form, are we going to put both initial and return trip modifiers (e.g., residence to dialysis would be RJ HCPCS modifier and residence to dialysis would be JR modifier) or would we utilize the modifier box 2 for the return trip modifier?
Answer: Suppliers should place both the origin and destination for both transports in the modifier 1 field (i.e., HCPCS modifiers RJ and JR); then use the modifier 2 field if they have a different origin or destination from modifier 1. Example: The beneficiary has to go to wound care in addition to dialysis. Use the Modifier 2 field to include the modifiers for the separate type of transport.
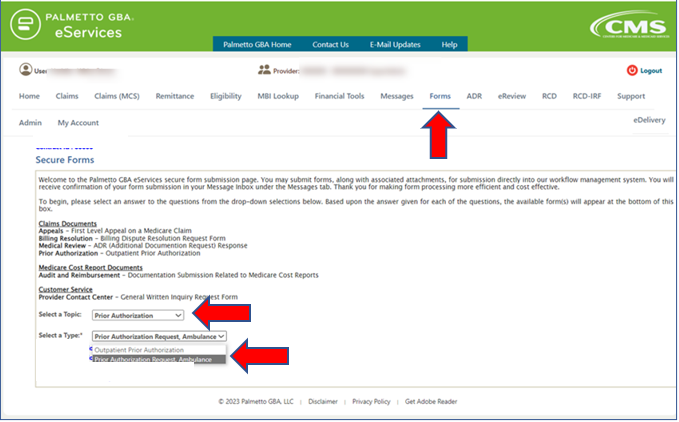
Question 47: How do we submit a Prior Authorization (PA) Request in eServices?
Answer: eServices users will access the form as follows:
- Navigate to the Forms tab
- Select Prior Authorization as the Topic
- Select the form link at the bottom Prior Authorization Request Form
- Complete the necessary fields
Question 48: I submitted an expedited Prior Authorization (PA) request. What happens if it does not qualify for expedited processing? Do I need to send another PA request?
Answer: No, you do not need to submit another request. If it is determined that the submitted information does not support expedited processing, your request will be moved to the regular PA request workload to be processed as normal. Detailed notes will be made in our system that can be checked by our Provider Contact Center (PCC).
Question 49: If I need to send another Prior Authorization (PA) request, how far in advance of the current PA expiration date can I send that?
Answer: The next PA request (if another 60-day period is needed) should not be submitted prior to day 45 into the current 60-day period (or about two weeks before the expiration date of the current PA).
Question 50: The prior authorization request I submitted was affirmed. Then I submitted a claim for the same beneficiary but for a non-repetitive service, so the Unique Tracking Number (UTN) was not included. Why did the claim reject asking for a UTN on a non-repetitive service?
Answer: The prior authorization program applies to all non-emergent (HCPCS codes A0426, A0428) ambulance transports, regardless of the origin or destination (National Expansion of the Repetitive, Scheduled Non-Emergent Ambulance Transport (RSNAT) Prior Authorization Model Fact Sheet, (PDF)). If the Medicare beneficiary has already met the criteria to establish that their ALS or BLS non-emergent transports are repetitive and a claim for a non-repetitive transport is submitted, this transport would count towards their number of affirmed transports. Submit the UTN on the claim. This will not permit the number of affirmed transports on that UTN to be exceeded.